Outbreaks of cyclosporiasis, an illness caused by the parasite Cyclospora cayetanensis, occur almost every year in the US, and this summer is no exception. People can become infected with Cyclospora by consuming food or water contaminated with the parasite. The outbreak beginning May 1, 2018, is an example of a typical outbreak. In this case, more than 206 laboratory-confirmed cases of cyclosporiasis were reported across eight states in the Midwest.
Source: CDC
Based on interviews with patients, investigators traced the outbreak back to bagged salad mix. The outbreak of Cyclospora infections highlights the importance of compliance with the Food and Drug Administration Produce Safety Rule and specifically worker health and hygiene principles.
Past Cyclospora Outbreaks in the US
Foodborne outbreaks of Cyclospora have been reported in the US since the mid-1990s and have been linked to various types of produce, including berries, herbs, and leafy greens.
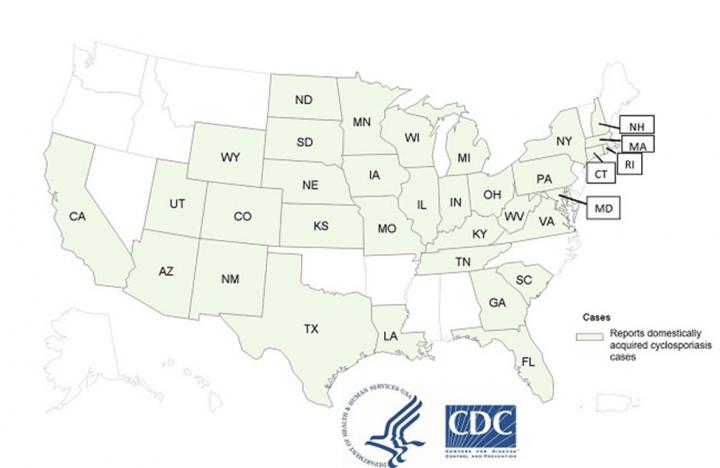
One of the most notable outbreaks of recent history was in 2019 when 2,408 laboratory-confirmed cases of cyclosporiasis were reported to CDC by 37 states, District of Columbia, and New York City in people who became ill between May 1 and August 31, 2019. At least 144 people were hospitalized; no deaths were reported. Multiple clusters of cases associated with different sources were investigated by State public health authorities, CDC, and FDA.
In September 2018, CDC was notified of 250 laboratory-confirmed cases of Cyclospora infections in people from four states who reported consuming pre-packaged vegetable trays containing broccoli, cauliflower, carrots, and dill dip. A separate cluster was reported to CDC in the same month, consisting of 511 infections in 15 states and New York City linked to the consumption of salads from a Midwest fast-food chain.
In the years between 2000 and 2017, there were at least 39 reported foodborne outbreak clusters of cyclosporiasis in the US. Over 1,700 people were infected across these 39 outbreaks. Berries were identified as the source of the in many of the early outbreaks.
How Cyclospora Infects Humans
Cyclospora’s life cycle and hosts are not fully understood. It is reported that in parts of Central America, Cyclospora infections may be endemic, meaning that there is normally some level of infection, but most people become immune. It is unclear if it is endemic in other regions. Those infected shed an “oocyst,” which is essentially an egg. When first excreted, the Cyclospora oocyst is not infectious. Once out of the host and in water or soil contaminated with fecal material, the oocyst becomes mature and capable of infecting a human host. The maturation process can take a week or more.
People become sick a week or more after consuming food or water contaminated with the mature Cyclospora oocyst. Infection through food appears to be more common than infection through drinking water. It is believed that those infected will develop an immunity that will prevent or reduce the severity of symptoms if infected again.
Diagnosis is made by microscopic examination and/or genetic testing of a fecal sample. Most people will fight off the parasite, but it can take a week or more. Symptoms of cyclosporiasis include malaise, fatigue, fever, muscle aches, and gastrointestinal symptoms including diarrhea and/or constipation, loss of appetite and weight loss, stomach cramps, nausea and vomiting, bloating, flatulence, and/or burping.
How Food Becomes Contaminated with Cyclospora
Food becomes contaminated when mature oocysts are present on the surface of food. This occurs when an infected person, usually a produce worker, uses a produce field to relieve themselves instead of using an approved sanitary facility, such as a portable restroom facility. The mature oocyst from the person’s feces may then contaminate the produce during weather events, irrigation, harvest operations, transportation, and/or washing. It’s important to note that inadequate handwashing after using a sanitary facility is not the only cause of food contamination.
How to Prevent Produce Contamination
Compliance with the FDA Produce Safety Rule (21 CFR §112) is important to prevent contamination of produce with Cyclospora. Some of the key elements of the rule involve employee health and hygiene, and of importance are those elements requiring employees to use approved bathroom/sanitary facilities. Due to incentives for harvest efficiency, employees may be tempted to save time by not using approved sanitary facilities and instead relieving themselves in the field. Supervisory employees have the responsibility to ensure workers are using approved sanitary facilities. This can be done by making the facilities convenient to the work location and giving workers adequate time to use the facilities without losing their efficiency incentives.
Employees can also be tested to verify they are not infected with the parasite. These tests are not complicated or time-consuming and can be performed by a public health laboratory. A course of antibiotics can be used to eliminate the parasite. Employees found to be shedding can be assigned tasks other than handling produce or closely supervised to ensure they use approved sanitary facilities.
Recent reports have implicated water used for irrigation, possibly contaminated with viable oocysts, could be a risk factor. If this water were to contacts the harvested portion of ready-to-eat produce, consumers could become infected. In addition, contaminated water used to clean and rinse product could also be a risk for contaminating the ready-to-eat product. Ensuring only potable water is used to clean produce is another essential risk-reduction step.
Testing Methods to Detect Cyclospora in Food and Water
After repeated outbreaks of Cyclospora, the FDA began developing a test to detect Cyclospora that was more sophisticated than previous methods. In 2015, FDA’s Center for Food Safety and Applied Nutrition (CFSAN) established a Foodborne Parasitology Research Program and tasked it with creating a new, more sensitive method to detect the parasite. The availability of this new method is a significant advancement in the FDA’s ability to investigate outbreaks of cyclosporiasis and identify the parasite in foods.
The FDA-developed Cyclospora detection test for fecal matter uses DNA extraction. A real-time polymerase chain reaction (PCR) test is then used to replicate and amplify the extracted Cyclospora DNA, which improves the sensitivity of the test. For food testing, FDA developed produce wash solutions that improve Cyclospora oocyst recovery and increase the likelihood of finding Cyclospora on a contaminated piece of produce.
The oocysts can then be tested using the DNA method described above. Additional work is needed to determine if the DNA linked to one outbreak is significantly different than the DNA linked to another outbreak. If the strains are different, more analysis will be required to determine if some strains are more common than others.
It is important to note that Cyclospora cayetanensis is not the only species of Cyclospora in the environment. There are species-specific Cyclospora that exist in nature that do not infect people. It is not clear if current testing methods for water and produce can differentiate the different species of Cyclospora in the environment. This has important regulatory implications.
Looking Ahead
The Centers for Disease Control and Prevention (CDC) and the Food and Drug Administration (FDA) have made attempts to better understand the factors contributing to Cyclospora infections. However, many cases of cyclosporiasis cannot be directly linked to an outbreak, in part because of the lack of validated molecular typing tools for Cyclospora cayetanensis.
New analysis methods are being evaluated that will allow an opportunity for differential diagnosis strains of Cyclospora if there is enough genetic diversity. This will enable a way to focus more quickly on illness clusters and more rapid traceback of food vehicles to production sites. This should allow for environmental assessments at production sites to determine routes of contamination and prevention option.
In the meantime, the best we can do is to emphasize the importance of compliance with the Food and Drug Administration Produce Safety Rule, and specifically worker health and hygiene principles and the water regulations.
Crisis24 provides in-depth intelligence, planning, and training, as well as swift and actionable responses to keep your organization ahead of emerging risks. Contact us to learn more.
Author(s)

Dr. Gary Weber
Senior Director, Food Safety and Contamination Prevention
Gary Weber is a U.S.-based Director of Food Safety and Contamination Prevention responsible for food production risk analysis and design of prevention measures. He joined Crisis24 in 2019, and holds...
Learn More